SHARES

Babies are normally in a headfirst position in the mother’s womb just before birth. Breech baby presentation is when the baby is lying feet first or bottom first in the womb (uterus). It is quite common in the early stages of pregnancy as most babies will turn into headfirst position by 36-37 weeks of pregnancy.
Occurring in 3% to 4% of term pregnancies, breech baby presentation is more common if it is the first pregnancy. In preterm labour, this occurrence can be as high as 43% at 32 weeks of gestation. 20% – 32.5% of breech presentation are undetected at term and these cases normally have worse outcomes. Recurrence rate of breech baby presentation is 9.9% if the previous pregnancy was also in breech presentation. In certain cases, breech presentation may be associated with uterine (womb) and congenital abnormalities.
What happens if indeed the baby did not turn into the headfirst position before birth?
In that case, here are options for breech baby delivery that your doctor may choose depending on what works best for each individual case.
Options for Breech Baby Delivery
- External cephalic version (ECV)
- Planned vaginal breech delivery
- Caesarean section
There are risks to be considered for each option and your doctor will advise accordingly the best option for your case.
1. External Cephalic Version (ECV)
External cephalic version is the manipulation of the baby, through the mother’s tummy, to a head down position. Overall, the success rate of ECV is approximately 50%. The success rate for first pregnancy is at approximately 40%, whereas for second pregnancy & above is at 60%. In cases when ECV is unsuccessful, there are only 3-7% of chances that the baby will subsequently turn to head down position spontaneously. If the ECV is successful, there is still 3% chance of baby turning back into breech position.
Generally speaking, ECV is more likely to be successful if:
- The current pregnancy is second pregnancy and above
- Baby’s buttock has not entered the pelvic inlet
- Medication is used to reduce contraction (tocolysis)
- Baby’s head is easily palpable through the abdomen
- Mother’s weight is of less than 65kg
- Placenta located at the back
- The baby is bottom first with both hips and knees flexed (complete breech)
- Adequate liquor / amniotic fluid
What is tocolysis?
Tocolysis is the reduction of uterine contraction with the use of medication. Commonly used medication is of betamimetic group and this will not be suitable for women with significant heart disease or high blood pressure. Common side effects of this medication include palpitations, flushing, tremor and nausea.
What are the contraindications for ECV?
- When the placenta separates early from the uterus (placental abruption)
- When the mother has high blood pressure with the presence of protein in the urine (severe pre-eclampsia)
- Abnormal baby’s umbilical blood flow (as demonstrable via ultrasound)
- Abnormal baby’s heartbeat pattern (as demonstrable on cardiotocograph, CTG).
- Multiple pregnancy
- Current or recent (within 1 week) vaginal bleeding
- When the water broke
- Any other reasons that require caesarean section
- Additional caution should be given to mothers with reduced amniotic fluid or high blood pressure.
Are there any risk with ECV?
Besides pain and discomfort, ECV carries a 0.5% risk of requiring emergency caesarean section within 24 hours. More than 90% of these cases will have vaginal bleeding or abnormal baby’s heartbeat pattern shown oncardiotocography (CTG).
Is ECV painful?
- 9% of women declined ECV for the fear of pain and vaginal birth
- 1/3 of women experienced significant pain
- 5% of women reported to have high pain scores
- 3/4 of women described ECV as uncomfortable
What else do I need to know about ECV?
- ECV should only be performed where facilities for monitoring and surgical delivery are available.
- There should not be more than 4 attempts of ECV.
- Overall procedure should ideally be within 10 minutes.
- Cardiotocography or CTG recording of the baby’s heartbeat pattern, is recommended prior and following ECV
2. Planned Vaginal Breech Delivery
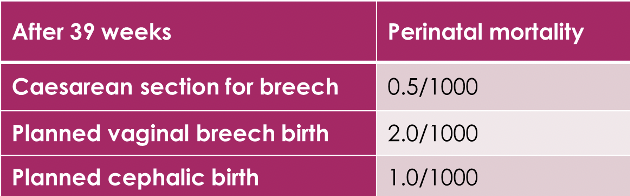
This option can be nearly as safe in selected pregnancies. But, it requires skilled healthcare professional with close monitoring throughout the labour. Even though it may increase the risk of short-term complication, there is no increase in the risk of long-term morbidity.
Planned Vaginal Breech Delivery is not suitable for:
- Baby with hyperextended neck, this can be detected by ultrasound
- Suspected big baby (more than 3.8kg)
- Suspected low birthweight (less than 10th centile)
- Baby with feet first position (footling breech)
- Fetal compromise or fetal distress
- Units with limited monitoring facilities or lack of experienced personnel
3. Planned Caesarean Section Breech Delivery
Caesarean section has its own associated risks. Common complications for instance, include wound discomfort, readmission to hospital, massive bleeding, infection and injury to the baby.
Mothers with previous caesarean section have a 25% chance of requiring a repeat caesarean section in subsequent pregnancy. Likewise, the more caesarean section a mother has, the higher the risk of subsequent pregnancy. One of the most feared complications is morbidly adhered placenta such as placenta accrete, increta or percreta.
Your doctor will individualise care for each case by considering the fertility wishes of the mother and other circumstances. There is no one rule that fits all.
References
Royal College of Obstetricians and Gynaecologists; 16/03/2017; External Cephalic Version and Reducing the Incidence of Term Breech Presentation (Green-top Guideline No. 20a)
Royal College of Obstetricians and Gynaecologists; 16/03/2017; Management of Breech Presentation (Green-top Guideline No. 20b)
Acknowledgement with thanks to Dr Tan Cheng who contributed this article.
For further information contact: Dr Tan Cheng, Tung Shin Hospital, Jalan Pudu, Bukit Bintang, KL – https://www.getdoc.com/en/clinic/tung-shin-hospital-o-g-dr-tan-5603
Dr Tan Cheng
MBChB (Bristol, UK), MRCOG (London, UK)
Consultant Obstetrician & Gynaecologist
Tung Shin Hospital, Jalan Pudu, Bukit Bintang, KL
If you need to consult an Obstetrician and Gynaecologist:
Find an Obstetrician and Gynaecologist in Malaysia, on GetDoc
Find an Obstetrician and Gynaecologist in Singapore, on GetDoc
Disclaimer
On balance, the authors, reviewers, and editors of GetDocSays have made extensive and reasonable efforts to ensure that medical information is accurate and conform to the standards of the publication. Also, they reflect the opinions and views of the contributors and not the publisher.
Likewise, the information on this site is not professional advice, neither to replace personal consultation with a physician, dentist, pharmacist, or other health care professional. Therefore the reader should not disregard medical advice or delay seeking it because of the information published here.
by Nashvini Rachel
View all articles by Nashvini Rachel.