SHARES

Antenatal Screening for Fetal Anomaly
Pregnancy is a joyful journey for majority of couples. One of the common questions during the antenatal follow up is whether the baby is normal. In this article we will go through a few questions about antenatal screening, focusing particularly on fetal anomaly.
What is Down syndrome?
Down syndrome is a chromosomal disorder. To begin with, each person has a genetic blueprint make up which we inherit from our parents. This blueprint is packaged in our cells in structures called chromosomes. Normally each of us has 46 chromosomes arranged in 23 pairs, 23 from the father and 23 from the mother. Down Syndrome is a common birth defect that is usually due to an extra chromosome 21 (Trisomy 21), a total of 47 chromosomes. Generally, it occurs most frequently in children born to mothers over age 35, the risk increases with maternal age.
What causes Down syndrome?
This genetic disorder is caused by an abnormal cell division where an extra partial or full copy of chromosome 21 occurs. In this case, the extra chromosome induces changes in fetal development, including the physical features seen in Down syndrome patients. As a rule, age is a big risk factor, as a mother gets older the chances of having a Down syndrome baby gets higher. See table below for co-relation between age and incidence:
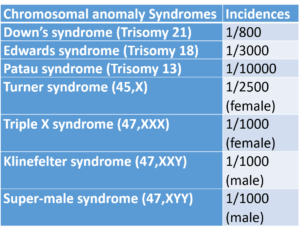
Other types of chromosomal disorder?
Yes, there are other types of chromosomal disorder such as
- Down’s syndrome (Trisomy 21)
- Edwards syndrome (Trisomy 18)
- Patau syndrome (Trisomy 13)
- Turner syndrome (45,X)
- Triple X syndrome (47,XXX)
- Klinefelter syndrome (47,XXY)
- Super-male syndrome (47,XYY)
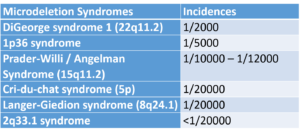
There are also other syndromes that are caused by micro-deletion (chromosomal deletion smaller than 5 million base pairs) spanning several genes. This is too small to be detected by conventional cytogenetic methods.
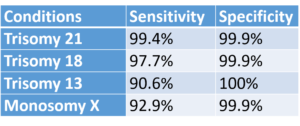
What are the incidences of chromosomal anomalies?
In summary, the 2 tables below show the incidences of the various anomalies.
What can we do to detect chromosomal anomalies?
Screening test will be the first line, initially. Here, screening test normally comes in the form of ultrasound scan and maternal blood test. Subsequently, if the screening test suggests high risk of chromosomal anomalies, your doctor will follow through with confirmatory diagnostic tests.
Ultrasound
Ultrasound is available since 1956, used during the first trimester to look at nuchal translucency and fetal nasal bone. In particular, increased nuchal translucency gives a 70-80% diagnosis of Down Syndrome, whereas, absence of nasal bone gives a 60-70% diagnosis of Down Syndrome. In addition, during the second trimester (between 18-21 weeks) a comprehensive ultrasound scan will be offered to look for structural anomaly of the baby, such as the baby’s heart.
Blood test
Serum markers are available since the 1980s. It can be used both in first trimester and second trimester to look at different markers in order to estimate the risk of anomaly.
First trimester serum markers: beta HCG, PAPP-A
Second trimester serum markers:
- Double test: AFP, total HCG
- Triple test: AFP, total HCG, serum estriol
- Quadruple test: AFP, total HCG, serum estriol, inhibin
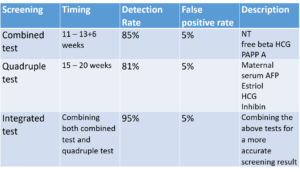
Traditionally, doctors offer a combined test between 11- 14 weeks of gestation. For instance, this consists of an ultrasound scan to look at nuchal translucency and nasal bone, together with a blood test to look at beta HCG, PAPP-A.
During second trimester, in between 15 – 20 weeks, doctors offer another blood test (Triple / Quadruple Test). This is to look at AFP, total HCG, serum estriol and inhibin.
Are there any new generation screening test?
Yes. The latest non-invasive screening test is the NIPT (non-invasive prenatal testing). It is a blood test and detects cell-free fetal DNA, to test for chromosomal anomalies (both chromosomal and micro-deletion). Since it is looking directly at the DNA, this test is far more accurate in comparison to the conventional methods (combined test, quadruple test and integrated test).
This test however is costly. It is at least 6x higher than the conventional screening methods.
What is the difference between screening test and diagnostic test?
Screening test is designed to estimate the risk of having a disease. Compared to the diagnostic test, screening test is non-invasive and carries less risk.
On the other hand, diagnostic test is invasive, normally requiring a small sample of the fetal tissue or the amniotic fluid.
If a screening test suggests a high risk of anomaly, the next step is to perform a diagnostic confirmatory test. So then, in between 11-14 weeks of gestation, chorionic villus sampling for confirmatory test may take place. In this case, tests involving chorionic villus sampling carry a 1-2% of miscarriage risk. Whereas, if the gestation is 15 weeks and above, amniocentesis can be done, with a 1% of miscarriage risk.
How do I know what is the best screening options?
During your first antenatal consultation, which is usually the longest consultation, your doctor will ask you a series of question to determine your risk. Subsequently, if your risk is high, your doctor will offer the screening test. Otherwise, if your risk is low and you are keen to proceed with the screening test, you may talk to your doctor to arrange for it.
In other developed countries such as United Kingdom, combined test and quadruple test are routinely offered to pregnant mothers. For the most part, NIPT test is used only as contingent screening.
Acknowledgement: We thank Dr Tan Cheng who contributed to this article.

Dr Tan Cheng
MBChB (Bristol, UK), MRCOG (London, UK)
Consultant Obstetrician & Gynaecologist
Tung Shin Hospital, Jalan Pudu, Bukit Bintang, KL
References:
- Caroline E Fox et.al. (2016) Prenatal diagnosis in the modern era; The Obstetrician & Gynaecologist; 2016; 18:213-9
- Fional L Mackie et.al. (2017) Cell‐free fetal DNA‐based noninvasive prenatal testing of aneuploidy; The Obstetrician & Gynaecologist; 2017; 19:211-218
- Gregg et al. (2016) Noninvasive prenatal screening for fetal aneuploidy, 2016 update: a position statement of the American College of Medical Genetics and Genomics. Genet Med 18(10), 1056-65
- NICE Clinical Guideline CG62 (February 2019) Antenatal care for uncomplicated pregnancies; National Institute for Health and Care Excellence
Tags
by GetDoc Team
View all articles by GetDoc Team.