SHARES

“When I fell sick with COVID-19, I was put into quarantine isolation to ring fence potential viral transmission. After my recovery, I am no longer infectious. So, I can go back to work knowing that I would not spread to others. However, will I get COVID-19 again?” Johnny, 36, wonders if recovery from COVID-19 would make him immune to the virus.
Is COVID-19 reinfection in patients who had recovered true? and what does that mean for immunity?
Immunity Against Viruses
Unlike living things, viruses are not made up of cells. This is because viruses, on their own, are unable to remain stable nor multiply nor make energy. Some biologists consider viruses non-living things, that can only replicate themselves by infecting other living cells.
During a viral infection, it takes about a week to 14 days for the human body to detect viruses hiding in our body cells. When that happens, the immune system kicks into gear to mass produce antibodies that target and kill these viruses. Therefore, most viral infection symptoms would start to subside after a week or so. This is the case for COVID-19 as well. That is why anyone with symptoms of COVID-19 would need to be isolated for 14 days to prevent viral spread.
On top of that, the human body’s immune system has great mechanisms to protect us from surrounding viruses that can even last for a lifetime. As a matter of fact, the body not only produces antibodies to kill the virus immediately, but also creates a large amount of stable and long-lasting antibodies to prevent further infection by the same strain of virus in the future. Furthermore, the body makes sure to keep a number of these antibodies-producing cells alive and continuously restock them whenever they age and die.
However even so, if the amount of long term antibodies that our body keep is insufficient to kill the invading virus, we can fall sick again to the same strain of virus. As this happens, our immune system learns to re-stock up a higher number of long-lasting antibodies so as to protect us from future infections. Sometimes, a single type of antibody can kill multiple strain of viruses. This is called cross-reactivity of antibodies.
Reinfection of COVID-19 in People Who have Recovered
Recently, a few reports appeared on cases of reinfection by COVID-19 after recovery. These are usually young people who had mild infection. Similarly, a number of studies also report the presence of viral particles in human faeces long after recovery. Having said so, there are still insufficient data to conclude if these observations are due to reinfection by COVID-19 or not.
On a cautionary note, these observations point out the need to re-evaluate our testing tools and strategies as well as our confidence in ruling out presence of COVID-19 viral infection. This is especially true for patients coming from epidemic zones with high risk of infection.
Possible Explanation for COVID-19 Reinfection
1. Sensitivity and Specificity of Testing Tools
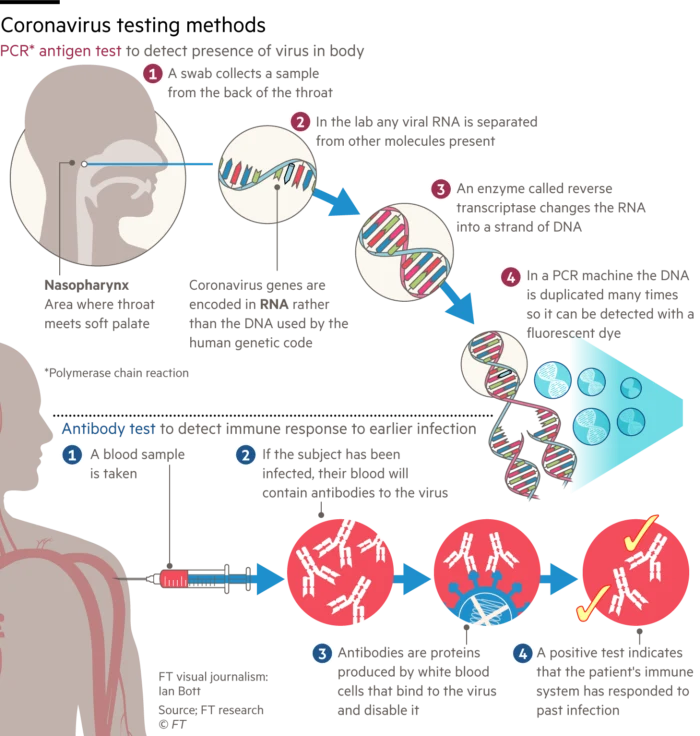
Most of the cases of suspected COVID-19 reinfection were tested negative first on commercial kits but subsequently tested positive with more sensitive tools like RNA detection method. This raises the question if these are cases of reinfection or false negatives due to lower sensitivity of commercial test kits.
By and large, the positive rate for nasal swab is about 63% for RNA testing within 7-10 days from symptoms onset. There remains room for discussion on the number of specimen collection from different sites and different time apart to increase accuracy of results.
2. Carrier State
Moreover, these patients may be in carrier state, where the body antibodies are just high enough for him or her to have no symptoms, but not enough to kill all the virus. Therefore, only with more sensitive tools are we able to detect the virus in patients under carrier state.
3. Specimen Error
To date, none of the close contacts of these suspected cases of reinfection fall sick nor test positive for COVID-19. There is still a possibility that these positive results may be due to wrong specimen collection technique, contamination of specimen, or specimen handling errors.
4. Possible Cross-reactivity of Antibodies
A rise in the number of antibodies against SARS-CoV-2 usually indicates an active infection of COVID-19. There is a possibility that the patient may be exposed to viruses that are similar to COVID-19 which cause the rise in antibodies. For instance, four strains of coronaviruses that cause common cold as well as MERS and SARS are all similar to SARS-CoV-2. These patients with common cold due to other strain of coronaviruses may be falsely labelled as positive for COVID-19.
5. Low Antibody Level
As described above, reinfection is possible if the stock of antibodies that our human body keep against COVID-19 is too low to prevent future infection. Research data are still insufficient to conclude on reinfection of COVID-19.
Conclusion
Few cases are pointing towards the possibility of COVID-19 reinfection in those previously recovered. However, there is still inadequate data to conclude on these observation. A number of factors such as testing tools, specimen handling and the nature of carrier state as well as cross-reactivity of antibodies may be the cause of these observations.
References:
1. Roy S. COVID-19 reinfection: myth or truth [PubMed]? SN Compr Clin Med. 2020 May 29: 1-4. doi 10.1007/s42399-020-00335-8.
2. “Immunity passports” in the context of COVID-19 [WHO]. WHO. 2020. (Available from: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19?gclid=Cj0KCQjwvvj5BRDkARIsAGD9vlJ9wT2FHF5jdR_02oDx8REI4kcLQkCm4HsQA8AsXmWOllwPY_6MEywaAnUQEALw_wcB; last updated on 2020 April 24; last accessed on 2020 Aug 21)
Find a GP/Family Doctor in Malaysia, on GetDoc
Find a GP/Family Doctor in Singapore, on GetDoc
by Chang Xian
View all articles by Chang Xian.