SHARES
Of late, we hear a term that is used very often – oh my thyroid levels are too low and that is the reason I am looking like this! Or sometimes, you also get to listen to “My thyroid levels are too high and it is affecting me more than I can imagine! What is it with these thyroid levels? What is the thyroid?
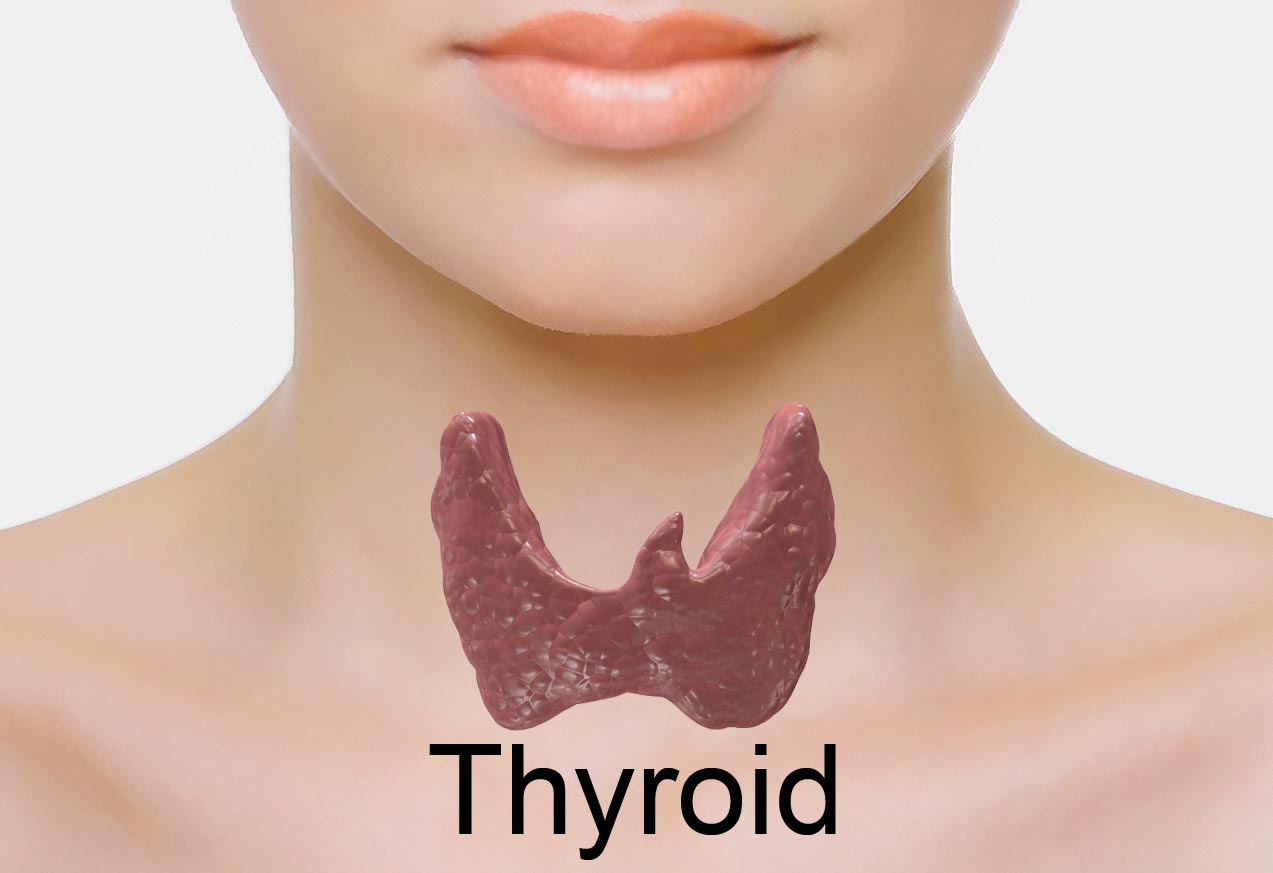
The “thyroid levels” or hormones are produced by the thyroid gland – a butterfly-shaped organ located at the base of the neck. It releases hormones called Thyroxine (T3, T4) that control metabolism—the way your body uses energy. The hormones produced by the gland, regulate vital body functions, such as breathing, heart rate, Central and peripheral nervous systems, body weight, muscle strength, body temperature, menstrual cycles, cholesterol levels and a lot more…
How does the Thyroid Gland Work
The thyroid is part of the endocrine system – made up of glands that produce, store, and release hormones into the bloodstream so these hormones can reach the cells in the body. The thyroid gland makes use of iodine from food we eat to make the 2 main hormones:
- Triiodothyronine (T3) & Thyroxine (T4)
It is important that the levels of T3 and T4 are maintained at optimum levels – neither too high nor too low. There are two glands located in the brain—the hypothalamus and the pituitary gland, which communicate to maintain T3 and T4 balance.
The hypothalamus produces a hormone called TRH (TSH Releasing Hormone) that signals the pituitary to tell the thyroid gland to produce more or less of T3 and T4 by either elevating or reducing the release of a hormone called thyroid stimulating hormone (TSH).
- When the levels of T3 and T4 are low in the blood, the pituitary gland releases more TSH to tell the thyroid gland to produce more thyroid hormones.
- If levels of T3 and T4 are high, the pituitary gland releases less TSH to the thyroid gland to bring down the production of these hormones.
What is the need for a Thyroid Gland
T3 and T4 travel in the bloodstream to reach almost every cell in the body. These hormones regulate the speed with which metabolism occurs. For example, T3 and T4 regulate the heart rate and how fast the intestines process food. So if the levels are low, heart rate may be slower than normal, and there could be constipation/weight gain. Whereas if the levels are high, it may lead to an opposite scenario – a rapid heart rate and diarrhoea/weight loss.
What could be the symptoms if one had too much of T3 and T4 in the body (Condition referred to as hyperthyroidism)?
- Sudden rapid weight loss
- Hand tremors
- Sweating
- Anxiety, nervousness
- High heart beat (tachycardia)
- Menstrual pattern change
- Fatigue
- Insomnia – inability to sleep
- Hair loss
Below is a list of symptoms when too little T3 and T4 are produced in the body (Condition referred to as hypothyroidism):
- Fatigue
- Constipation
- Unexplained and excess weight gain
- Muscle ache, tenderness
- Irregular menstrual periods (heavy)
- Hair loss
- Lowered heart rate
- Swollen neck region
How is the level of Serum Thyroid Hormone measured?
- Radioimmunoassay for T3 and T4
- Thyroid Binding Globulin measurement
- Measurement of Pituitary Production of TSH
- Iodine uptake scan
- Measurement of TRH
- Scans of thyroid gland
There has been a surge in the number of thyroid abnormalities in case women who have just delivered. In the postpartum period, women are seen to experience many changes in their body – problems of fatigue, pain from a C section or episiotomy, anaemia etc. Fatigue is especially common because of frequent waking – late night feeds and the continuous responsibilities of a new baby. Baby blues commonly occur and so is post-partum depression. These complications usually occur soon after the baby is born, and by, say the third month after delivery most women are feeling alright again. Unfortunately, this is not true in case of all women; some of them do not enjoy a quick return to good health. For many of them, the cause may be related to a change in thyroid function after delivery.
Why Does It Happen?
During pregnancy, the immune system is suppressed as a protection for the baby. After delivery there is a marked increase in immune activity and sometimes it worsens into immune conditions such as disease of the thyroid gland and rheumatoid arthritis. Although thyroid dysfunction may occur any time after pregnancy, it is most common about two to three months after delivery. However, by that time, visits to the obstetrician may have ended if it was an uneventful pregnancy and delivery.
Anyone with the symptoms of an overactive or underactive thyroid or postpartum depression should have a TSH test to predict whether thyroid levels are normal. The levels of thyroid hormone need not be checked unless the TSH is high (which indicates hypothyroidism) or low (which indicates hyperthyroidism).
This condition is called postpartum thyroiditis. It is a general term that refers to the inflammation of the thyroid gland that occurs in women after a delivery. Thyroiditis can cause both hypothyroidism (low thyroid hormone levels in the blood) and thyrotoxicosis (high thyroid hormone levels in the blood). In postpartum thyroiditis, it is seen that thyrotoxicosis occurs first followed by hypothyroidism.
Postpartum thyroiditis – what is its cause?
The exact cause is not known but it is believed to be an autoimmune disease quite similar to Hashimoto’s thyroiditis. In fact, these two disorders cannot be distinguished from one another on pathology specimens. As in the case of Hashimoto’s thyroiditis, postpartum thyroiditis is associated with the development of anti-thyroid (anti-thyroid peroxidase, anti-thyroglobulin) antibodies. Women with positive anti-thyroid antibodies are at an increased risk of developing postpartum thyroiditis than women who do not have positive antibodies. It is believed that women who develop postpartum thyroiditis have an underlying asymptomatic autoimmune thyroiditis that flares in the postpartum period when there are fluctuations in immune function.
Treatment:
Standard treatment for hypothyroidism – Daily use of the synthetic form of the thyroid hormone levothyroxine. This oral medication restores adequate hormone levels, thereby reversing the signs and symptoms of hypothyroidism.
For patients with sustained forms of hyperthyroidism, such as Graves’ disease or toxic goiter, anti-thyroid medications are often used. The goal with this form of drug therapy is to prevent the thyroid from producing hormones. Radioactive iodine is the most widely-recommended permanent treatment of hyperthyroidism. Surgical removal of the gland is another permanent cure.
Reference:
by Hridya
A biochemist by education who could never put what she studied to good use, finally found GetDoc as a medium to do what she loved - bring information to people using a forum that is dedicated to all things medical. View all articles by Hridya.





